Whilst this video is of a specific pelvic device, the principles apply equally in our setting. And hopefully we can arrange a station visit by Sam Medic…
NSW Ambulance Pelvic Binding Skill Sheet:
Aim:
To reduce a pelvic fracture, provide mechanical stability to the pelvis, and reduce blood loss.
Indication
All trauma patients with any of the following
• signs of a pelvic fracture including pain in the pelvis, hip, groin or lower back; or
• signs of hypovolaemic shock; or
• suspicious mechanism of injury, even if currently haemodynamically stable
The application of pelvic sheeting has negligible adverse effects on those patients who are subsequently found did not sustain a pelvic fracture.
Applying it to fifty patients who didn’t need it is worth it for the one who does
High risk groups include:
• Motor vehicle crashes, especially with patient side impact
• Vehicle v pedestrian / cyclist
• Motor bike crash
• Crush or compressive force
• Patients > 65 years of age
• Fall from height
• Fallen from, trampled or crushed by livestock
Have an increased index of suspicion with:
• Patients with decreased level of consciousness
• Drug or alcohol affected
• Significant distracting injury
Pelvis MUST NOT be sprung or compressed, however pelvis should be gently palpated as part of
patient assessment.
ALWAYS apply pelvic sheeting when indicated, even in urgent transport situations.
Blood loss from pelvic fracture can exceed 2 litres – this needs to be mitigated as the highest priority to
prevent worsening shock.
Every 3 minutes of untreated hypotension causes mortality to rise by 1%.
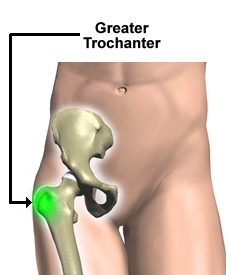
Some guidamce on placement of the pelvic sheeting:
Evidence based discussion on prehospital management of Pelvic trauma:
24232012_ The prehospital management of pelvic fractures_ initial consensus statement
17251627_ The prehospital management of pelvic fractures
Main points from the literature review and consensus statement:
– A binder is a treatment not a packaging tool, apply it early.
– A pelvic binder should be applied prior to extrication.
– Log rolling should be avoided and a scoop used where possible, rolling only to 15 degrees to facilitate placement on the board.
– Binder should be placed as close to skin as practical.
– There is a high incidence of occult pelvic fracture and bleeding in the obtunded major trauma patient(76%), so a high index of suspicion should be maintained, and a binder considered whenever a collar is placed due to mechanism.
– Up to 35% of total blood volume can be lost into the pelvis before any change is noted in systolic blood pressure. Permissive hypotension should be practised, with the presence of a radial pulse being the endpoint for fluid resus in the blunt trauma patient with no closed head injury.
– Examination is unreliable, springing has been shown to have a sensitivity of only 59%. Combined with the risk inherent of exacerbating haemorrhage this procedure has no role in pelvic injury assessment.
This is a great video on the bleeding associated with pelvic fractures, watch just the first minute.:
Following are some resources on the T-Pod, a pelvic binding device used by SOT. The T-Pod is employed as it is light, can be applied by one operator and is useful in the setting of deployments and remote work. It is carried by SOT responders in all situations however it is primarily for use in remote or deployment environments. The following is some information on the device to gain some familiarity as you may see it around, Careflight 4 also use the T-Pod in Sydney.
This is a “mini” systematic review of the literature to assimilate evidence when there is not a huge amount of literature available. Findings are that pelvic binding devices commercially available all reduce pubic symphisis diastasis significantly:
Emerg Med J-2013-Best Evidence Topic Reports-424-5
A case series report showing application of the T-Pod reduces heart rate, increases blood pressure and reduces pelvic volume in trauma patients with unstable pelvic fractures. 15 patients included:
Tan-TPOD-en-bekkenfractuur-Injury-2010
X-ray demonstration of the effect of the T-Pod on an open book pelvic fracture:
And lastly just a couple of newly published papers that you might be interested in checking out:
23962031_ Prehospital use of cervical collars in trauma patients_ a critical review
24972965_ Bag ’em or tube ’em_ how to decide
24210369_ Primary percutaneous coronary intervention for refractory cardiac arrest